
Discover the importance
of blood platelets!
Find out what one trillion
defenders in our blood do and why.
Platelets — One trillion defenders in our blood.
Welcome to plateletMAP™, an interactive site where you can learn about platelet interactions and functions in the body, ask questions, contribute knowledge and build a network!
Few people know that platelets are immune cells. They constanty survey the body for disturbances in the blood. Examples of disturbances are microorganisms or chemicals that should not be in the blood which could be a consequence of leaky gut. Temperature outside the physiological range, and wounds are other examples of disturbances. When platelets encounter disturbances they activate. This means that platelet activation is an indicator of stress in the body. Thus, chronic leaky gut is constantly challenging the immune function of platelets that causes chronic platelet activation. In other words, activated platelets signal this disturbance in the body.
This is why I call platelets our trillion defenders in the blood. Healthy life style choices reduce the disturbances in the body, giving platelets fewer reasons to activate. This is how you can take responsibility of your health!
Platelet Development
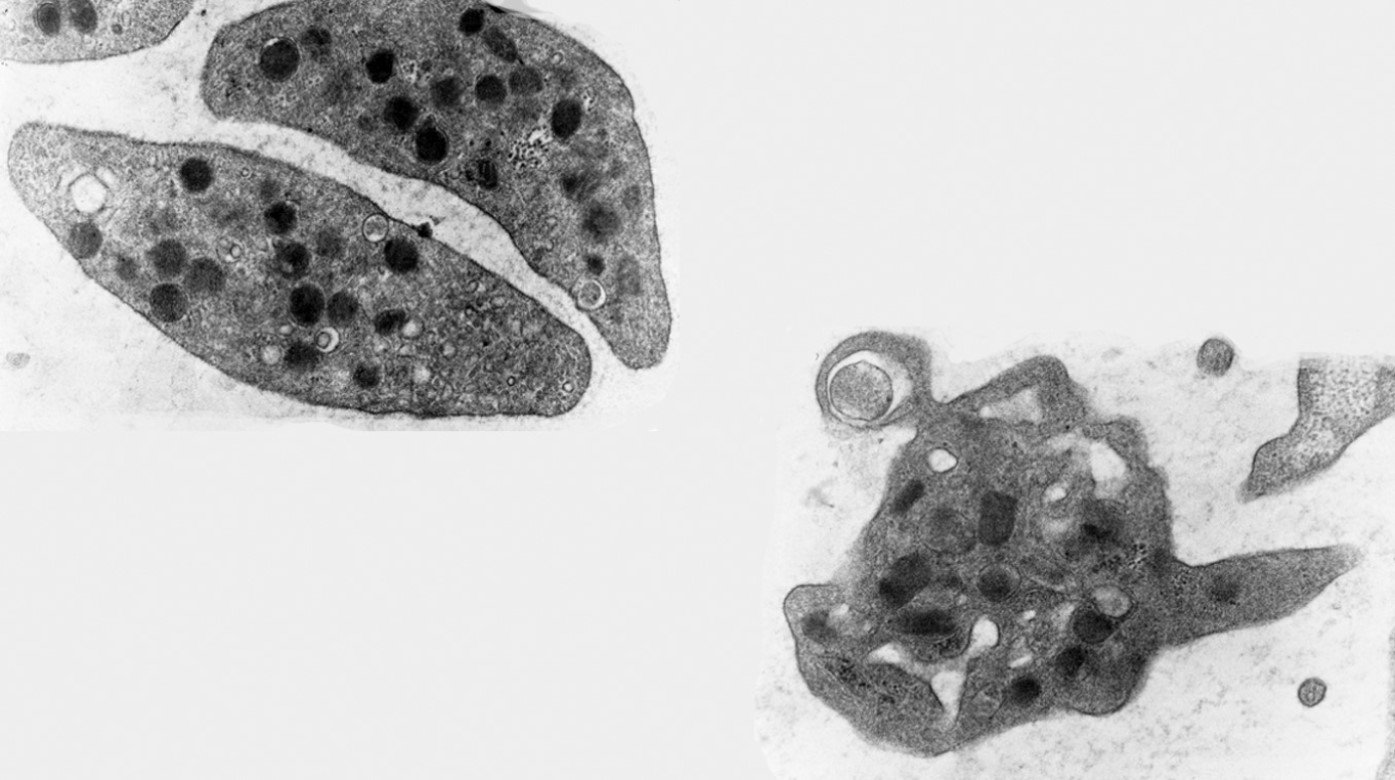
Platelets are produced by cells in the bone marrow called megakaryocytes. By default, platelets are created in their resting, discoid state. [1]
Platelets are a mammalian specialty. They evolved and specialized from amebocytes (e.g., horseshoe crab) to thrombocytes (e.g., bullfrog) to serotonin-containing thrombocytes in warm-blooded animals [2] and finally, anucleated blood platelets in mammals (see blog The secret lives of platelets).
Platelet Function
A person has typically 1 trillion platelets circulating in their blood. This number is based on an average blood volume of 5 liters and an average platelet count of 200,000 per microliter. To prevent or stop bleeding a much lower number would normally suffice suggesting that platelets have an additional function.
Microbes in the nose, mouth, gut, and on the skin defend defend the human body against foreign substances or pathogens from the outside. If the microbiota are not successful and foreign substances or pathogens get into the blood, platelets are the non-specific, first line defenders in the blood. Platelets are innate immune cells [3, 4].
Platelets are also hemostatic/clot forming cells which means they prevent and stop bleeding by filling holes in blood vessels.
When platelets perform their immune and hemostatic functions they use cellular mechanisms known as platelet activation. Both resting and activated states of platelets are natural and necessary when platelets fulfill their roles as immune cells and hemostatic cells. Resting and activated platelets perform their immune and hemostatic functions differently which is illustrated by plateletMAP with the example of leaky gut.
Resting platelet
What is platelet activation?
PLATELET ACTIVATION IS A NECESSARY DUALISM.
Platelets activate in response to stress, i.e., platelet activation indicates a disturbance in the body (see blog The truth about "bad" platelets).
When platelets activate they change their shape, their surface characteristics, and fragment into microparticles. By releasing microparticles or substances such as serotonin, platelets communicate with other cells and other parts of the body. These changes can all be measured to determine the activation state of platelets.
Activated platelet
WHAT LEADS TO PLATELET ACTIVATION?
Platelets are extremely sensitive. They activate at temperatures below 30°C and above 42°C, in response to high shear forces, pathogens, and many chemicals (see blog Why are they called blood platelets?).
This is necessary for their role as defenders of the body. Wounds and leaky gut are also types of stress that lead to platelet activation.
Platelets in the blood of patients suffering from depression are highly activated and contain only half the normal serotonin level, suggesting that leaky gut and depression are directly connected.
Suspended in blood — Platelets reach all parts of the body.
In every blood vessel platelets stop bleeding and defend the body against foreign substances and pathogens.
Megakaryocytes produce platelets in the bone marrow.
New platelets take up serotonin which is produced in the gut.
Activated platelets are removed in the spleen or in the liver.




